I had an email from the BTLP-TACT people today. I was a tad miffed to read “… you may need to complete further TACT participations to improve your
engagement target with the system” when I’m told by all of my colleagues that I do far more exercises than they do, and that they don’t get these reminders.
The last time I did one was two weeks and one day ago. How often am I supposed to do these? But it is good CPD, and it is free…
I
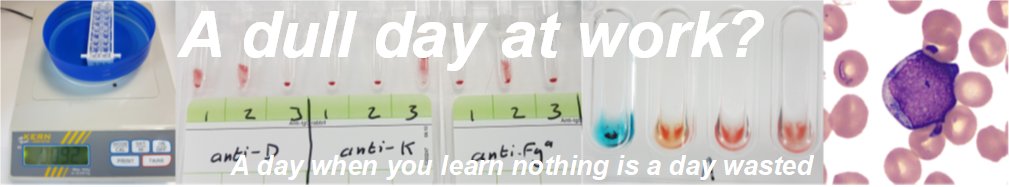
was presented with one case; a twenty-two year-old woman needing two
units of irradiated blood within the next two hours. She typed as O Pos
with a negative antibody screen. I selected
two units of O Pos irradiated blood (both of which were K-negative)… and
got the green light.