Here’s a case
study close to home… this happened to me in the middle of the night at the end
of last week…
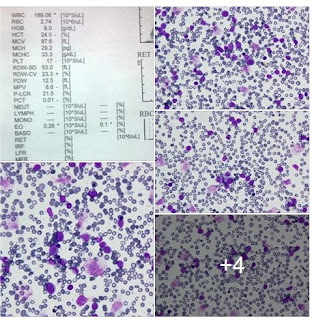
A patient presented
just before midnight with low Hb and with a GI bleed. Male, in his seventies,
and with no transfusion history. Units of blood were requested…
As there was
no history I insisted on having two blood samples taken at different times. Cell
groups presented as A Rh(D); however the reverse groups presented as O. Agglutination
was seen in both A and B cells. Antibody screens in both samples were negative.
My immediate reaction
was that this was a case of A2 with an anti A1. However
with no anti A1 available I was unable to confirm this. But this
theory went out the window when two of the four units of blood I crossmatched
were clearly incompatible.
I did
photograph the antibody panel; I wish I knew what I did with the picture. But
suffice it to say the results were incredibly inconclusive. By now it was 3am
and I was just a little bit worried.
I had another
look at the antibody panel and realised something. Reactions had occurred in
cells that were all homozygous for the M antigen. Anti-M would explain what was
going on. But lacking any anti-M reagent I was unable to confirm the M-status
of the supposedly compatible units. They could well have been heterozygous and
test compatible but could cause a reaction.
I spoke to
the doctors and explained the situation. I had two units which might be
compatible, but I couldn’t be sure.
The patient
was stable, and we arranged for further samples to be taken to be sent to the
reference lab, and for M-negative units to be supplied from the NBS.
Now (a few days later) I’m told I did the right
thing(s). But I can’t help but wonder
where the anti-M came from… and what would I have done if they had insisted on
transfusing him?